H1N1 and Vaccine Update
Influenza-like illnesses (ILIs) accounted for 3.2% of outpatient visits during week 51 that ended December 26. This is an increase from 2.3% a week ago.
All influenza A isolates during the week of December 20-26 were 2009 influenza A (H1N1). Analysis of recent strains showed that 99.7% are related to the H1N1 vaccine strain.
Vaccine for 2009 influenza A is now readily available in most places in the United States. The total number of doses available as of December 30, 2009 was 118 million doses. About half of the states now offer this vaccine to people who are not in the high-risk groups, and many states are now using pharmacies to facilitate distribution.
Resistance tests completed on 2445 strains of 2009 influenza A (H1N1) found that 38 (1.6%) were resistant to oseltamivir; 34 of 36 patients with resistant strains were from patients with documented exposure to oseltamivir.
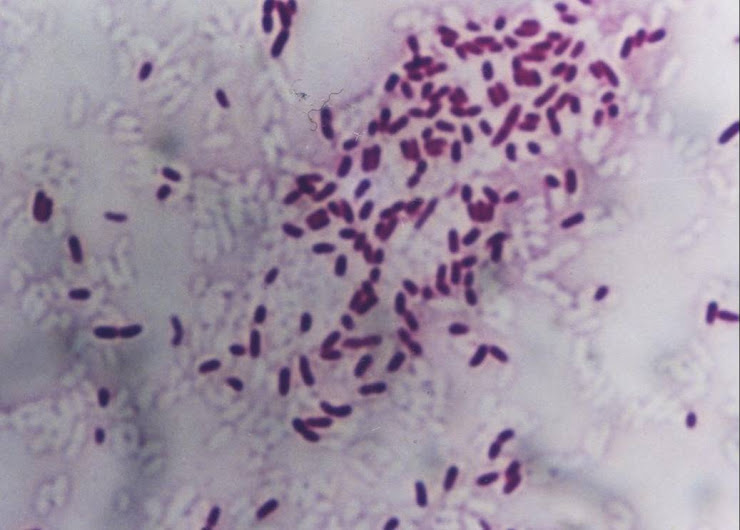
The total number of pediatric deaths attributed to 2009 influenza A (H1N1) since August 20, 2009 is 225. Reviews of 106 of these cases indicate bacterial superinfection in 35 (33%) patients, including Streptococcus pneumoniae in 10 patients and Staphylococcus aureus in 10 patients.
Influenza-like illnesses (ILIs) accounted for 3.2% of outpatient visits during week 51 that ended December 26. This is an increase from 2.3% a week ago.
All influenza A isolates during the week of December 20-26 were 2009 influenza A (H1N1). Analysis of recent strains showed that 99.7% are related to the H1N1 vaccine strain.
Vaccine for 2009 influenza A is now readily available in most places in the United States. The total number of doses available as of December 30, 2009 was 118 million doses. About half of the states now offer this vaccine to people who are not in the high-risk groups, and many states are now using pharmacies to facilitate distribution.
Resistance tests completed on 2445 strains of 2009 influenza A (H1N1) found that 38 (1.6%) were resistant to oseltamivir; 34 of 36 patients with resistant strains were from patients with documented exposure to oseltamivir.
The total number of pediatric deaths attributed to 2009 influenza A (H1N1) since August 20, 2009 is 225. Reviews of 106 of these cases indicate bacterial superinfection in 35 (33%) patients, including Streptococcus pneumoniae in 10 patients and Staphylococcus aureus in 10 patients.
Commentary. What does this mean for practitioners?
The second wave of H1N1 is resolving, although the total ILI reports for week 51 were higher than for week 50: Nationally we are nearly back to baseline rates of ILI.
There is now plenty of 2009 influenza A vaccine: In fact, the US Centers for Disease Control and Prevention (CDC) has launched a big promotional campaign to encourage vaccination.
What will happen in January-March 2010 when seasonal flu usually hits? No one knows, but there are 3 possibilities: (1) seasonal flu will circulate as usual, with influenza A (H1N1 and H3N2) plus influenza B; (2) seasonal flu will occur with the pandemic 2009 influenza (H1N1) strain predominating; or (3) no flu will occur. Of note, seasonal flu strains are not evolving much in the world. Thomas Freiden, MD, MPH, Director of the CDC, asked 12 world influenza experts to predict what is going to happen with regard to influenza. Half of the experts said that there would be a third wave of pandemic (H1N1) flu, and half claimed that there would not be a third wave. In the southern hemisphere where the winter season ended in September, the 2009 influenza A (H1N1) strain "pushed out seasonal flu," and thus far Europe and the United States are almost exclusively finding the pandemic strain. In previous influenza pandemics (1918, 1957, and 1968) the pandemic strain also dominated in flu season. However, no one is confident enough to predict what will happen, in large part because the influenza virus continues to defy predictions.
There is now plenty of 2009 influenza A vaccine: In fact, the US Centers for Disease Control and Prevention (CDC) has launched a big promotional campaign to encourage vaccination.
What will happen in January-March 2010 when seasonal flu usually hits? No one knows, but there are 3 possibilities: (1) seasonal flu will circulate as usual, with influenza A (H1N1 and H3N2) plus influenza B; (2) seasonal flu will occur with the pandemic 2009 influenza (H1N1) strain predominating; or (3) no flu will occur. Of note, seasonal flu strains are not evolving much in the world. Thomas Freiden, MD, MPH, Director of the CDC, asked 12 world influenza experts to predict what is going to happen with regard to influenza. Half of the experts said that there would be a third wave of pandemic (H1N1) flu, and half claimed that there would not be a third wave. In the southern hemisphere where the winter season ended in September, the 2009 influenza A (H1N1) strain "pushed out seasonal flu," and thus far Europe and the United States are almost exclusively finding the pandemic strain. In previous influenza pandemics (1918, 1957, and 1968) the pandemic strain also dominated in flu season. However, no one is confident enough to predict what will happen, in large part because the influenza virus continues to defy predictions.
Should your patients still get vaccinated? The CDC estimates that about one sixth (15%) of the population of the United States has had influenza, meaning that 85% have not contracted it yet. Their recommendation is for vaccination for both seasonal and pandemic flu—a single dose of each at separate injection sites for people older than 9 years of age and 2 doses separated by 4 weeks for children 6 months to 9 years of age. The original priority groups are still the highest priority for vaccination. The assumptions here are that there will be a flu season, but we cannot predict the strain(s) that will be responsible for it. Only time will tell whether this is sage advice. Of interest, President Barack Obama, First Lady Michelle Obama, and daughters Malia (11 years) and Sasha (8 years) have all received the H1N1 vaccine. The president said he knows that the vaccine is safe.[3]
2009 H1N1 Flu Virus Outbreaks in Animals[4]
Reports from the American Veterinary Medicine Association summarize the available data on 2009 influenza A (H1N1) in domestic animals and livestock:
Cats: 11 cases (Pennsylvania-1, Oregon-6, Colorado-2, Utah-1, Iowa-1) have been reported to have influenza; 8 were virologically confirmed; 4 deaths have occurred; and in 6 cases a human source was identified. One cat was stated to have chronic sinusitis and was treated with oseltamivir, but subsequently died.
Ferrets: 13 cases reported (Nebraska-4, Oregon-9); 1 death.
Dogs: 1 case reported (New York). This dog recovered after 2 days of hospitalization. The Chinese press has also reported 2009 H1N1 in dogs.
Turkeys: An outbreak occurred in a Virginia flock following contact with a human case. A second outbreak occurred later on the same Virginia farm, and positive tests have been reported in turkeys with surveillance cultures in Illinois, Canada, and Chile.
Cheetahs: 4 cheetahs in a cluster of respiratory illnesses occurred in a California zoo. The animals presented with harsh coughs, tachypnea, and rough haircoats. One case was virologically confirmed. All animals recovered in 5-16 days.
Pigs: 12 outbreaks have been reported in Indiana and Minnesota in the United States as well as in Germany, England, Indonesia, Taiwan, Canada, Argentina, Singapore, Ireland, Norway, and Japan. The US Department of Agriculture (USDA) Agricultural Research Service has confirmed that meat tissue from infected pigs does not contain the virus at 3, 5, or 7 days after exposure, and pork is not considered a foodborne threat. The USDA has a conditional license for a 2009 H1N1 influenza vaccine for pigs.
2009 H1N1 Flu Virus Outbreaks in Animals[4]
Reports from the American Veterinary Medicine Association summarize the available data on 2009 influenza A (H1N1) in domestic animals and livestock:
Cats: 11 cases (Pennsylvania-1, Oregon-6, Colorado-2, Utah-1, Iowa-1) have been reported to have influenza; 8 were virologically confirmed; 4 deaths have occurred; and in 6 cases a human source was identified. One cat was stated to have chronic sinusitis and was treated with oseltamivir, but subsequently died.
Ferrets: 13 cases reported (Nebraska-4, Oregon-9); 1 death.
Dogs: 1 case reported (New York). This dog recovered after 2 days of hospitalization. The Chinese press has also reported 2009 H1N1 in dogs.
Turkeys: An outbreak occurred in a Virginia flock following contact with a human case. A second outbreak occurred later on the same Virginia farm, and positive tests have been reported in turkeys with surveillance cultures in Illinois, Canada, and Chile.
Cheetahs: 4 cheetahs in a cluster of respiratory illnesses occurred in a California zoo. The animals presented with harsh coughs, tachypnea, and rough haircoats. One case was virologically confirmed. All animals recovered in 5-16 days.
Pigs: 12 outbreaks have been reported in Indiana and Minnesota in the United States as well as in Germany, England, Indonesia, Taiwan, Canada, Argentina, Singapore, Ireland, Norway, and Japan. The US Department of Agriculture (USDA) Agricultural Research Service has confirmed that meat tissue from infected pigs does not contain the virus at 3, 5, or 7 days after exposure, and pork is not considered a foodborne threat. The USDA has a conditional license for a 2009 H1N1 influenza vaccine for pigs.
Commentary. Most cases in pets have been associated with human index cases, and none of these cases were known to represent human disease following animal exposure. The obvious exception is the index case of pig-to-human transmission that occurred at some unknown time and place. Veterinarians maintain that this is a veterinary health issue and not a human health issue. Most of the pets presented with fever, cough, and lethargy. People with flu who have dogs, cats, or ferrets are advised to wash their hands, sneeze into their sleeves, and practice "social distancing" to protect pets. A diagnostic test for the H1N1 virus in pets is available from Innovative Diagnostics and Technologies (IDEXX) laboratories.
Virus of the Year: The Novel H1N1 Influenza[5]
For years, scientists have warned about a pandemic of influenza that might be similar to the 1918 Spanish flu pandemic that is considered the worst epidemic in recorded medical history with 50-100 million deaths, but:
It was supposed to come from Asia: Instead, it came from North America;
It was supposed to be a new strain like avian flu (H5N1): It was simply another form of H1N1;
It was supposed to be severe with high lethality: It was severe in some unpredictable populations, such as children and pregnant women, but overall mortality was only about 0.2%-0.04%; and
It was supposed to cause catastrophe: Instead, it caused confusion.
A Cluster of Oseltamivir-Resistant H1N1 Influenza Cases[6]
This report concerns 10 students in Vietnam who shared a 42-hour train journey. These students did not know each other prior to the journey, and none had known contact with a person with influenza prior to the journey. None of the students were symptomatic during the journey, but 7 developed influenza symptoms within 48 hours after the journey. All 7 of these students had positive reverse-transcriptase polymerase chain reaction (RT-PCR) tests for influenza A (H1N1), and all 7 strains had the H275Y substitution that confers resistance to oseltamivir. None of the students had previously received oseltamivir. Six of the 7 students were hospitalized for isolation and 1 student was isolated at home. No additional cases were identified from this cluster.
Virus of the Year: The Novel H1N1 Influenza[5]
For years, scientists have warned about a pandemic of influenza that might be similar to the 1918 Spanish flu pandemic that is considered the worst epidemic in recorded medical history with 50-100 million deaths, but:
It was supposed to come from Asia: Instead, it came from North America;
It was supposed to be a new strain like avian flu (H5N1): It was simply another form of H1N1;
It was supposed to be severe with high lethality: It was severe in some unpredictable populations, such as children and pregnant women, but overall mortality was only about 0.2%-0.04%; and
It was supposed to cause catastrophe: Instead, it caused confusion.
A Cluster of Oseltamivir-Resistant H1N1 Influenza Cases[6]
This report concerns 10 students in Vietnam who shared a 42-hour train journey. These students did not know each other prior to the journey, and none had known contact with a person with influenza prior to the journey. None of the students were symptomatic during the journey, but 7 developed influenza symptoms within 48 hours after the journey. All 7 of these students had positive reverse-transcriptase polymerase chain reaction (RT-PCR) tests for influenza A (H1N1), and all 7 strains had the H275Y substitution that confers resistance to oseltamivir. None of the students had previously received oseltamivir. Six of the 7 students were hospitalized for isolation and 1 student was isolated at home. No additional cases were identified from this cluster.
Commentary. During the 2008-2009 influenza season, a sudden development of oseltamivir resistance occurred in the seasonal influenza A (H1N1) strains, increasing resistance from <> 98% in most areas of the world, including the United States. This change in resistance pattern was unrelated to oseltamivir use. So far, > 98% of pandemic 2009 influenza A (H1N1) strains have been sensitive to oseltamivir, and nearly all resistant strains have been associated with prior oseltamivir use. This cluster of cases in Vietnam demonstrates how a dramatic change in oseltamivir sensitivity without oseltamivir use is possible, which explains the reason for close watching of the new pandemic strain.
Diagnostic Testing for 2009 Influenza A (H1N1) Virus in Hospitalized Patients[7]
RT-PCR is the most sensitive test;
The problem with rapid diagnostic tests and immunofluorescence assays is false-negative results;
The best specimens are nasopharyngeal swabs, aspirates or washes, or nasal and throat swabs tested as early in the infection as possible; and
Some patients with negative RT-PCR tests from nasopharyngeal specimens have had positive RT-PCR tests from endotracheal aspirates or bronchoalveolar lavage specimens.
RT-PCR is the most sensitive test;
The problem with rapid diagnostic tests and immunofluorescence assays is false-negative results;
The best specimens are nasopharyngeal swabs, aspirates or washes, or nasal and throat swabs tested as early in the infection as possible; and
Some patients with negative RT-PCR tests from nasopharyngeal specimens have had positive RT-PCR tests from endotracheal aspirates or bronchoalveolar lavage specimens.
Commentary. The last bulleted point above is relatively new and important information for clinicians. The pandemic strain of influenza binds to the lower airway cells, and this apparently accounts for positive endotracheal aspirates after the upper nasopharyngeal infection has cleared.
Clinical Features of the Initial Cases of 2009 Pandemic Influenza A (H1N1) Virus in China[8]
The study concerned 426 travelers with confirmed influenza who were quarantined in 61 hospitals in China. Cases were detected by thermal screening at airports and by contact tracing. The mean patient age was 24 years: Five percent were white; 43% had recently traveled to the United States; and 41% had airplane exposure. Results of interest include the following:
Of 56 million travelers screened
17,909 had fever and a respiratory illness
757 (14 per million) had influenza with the 2009 influenza A (H1N1) strain
Lab tests showed
C-reactive protein > 10 mg/L (31%)
Median CD4 count, 576 cells/µL
White blood cell (WBC) count > 10,000/mm3 (3%)
Mean WBC count, 3440/mm3
Total lymphocyte count, < 15,000/mm3 (68%)
Abnormal chest x-ray (5%) with "patchy infiltrates" in 12 of 14
Abnormal chest computed tomographic (CT) scan (7%)
Symptoms included
Fever (67%)
Cough (70%)
Sputum production (25%)
Sore throat (37%)
Diarrhea (3%)
Nausea (2%)
Viral shedding
Mean of 6 days by RT-PCR
Mean of 3 days after becoming afebrile
Longer with age < 14 years (odds ratio [OR] 1.94)
Longer with delayed oseltamivir treatment (> 48 hours after onset of symptoms [OR 4.5]).
Clinical Features of the Initial Cases of 2009 Pandemic Influenza A (H1N1) Virus in China[8]
The study concerned 426 travelers with confirmed influenza who were quarantined in 61 hospitals in China. Cases were detected by thermal screening at airports and by contact tracing. The mean patient age was 24 years: Five percent were white; 43% had recently traveled to the United States; and 41% had airplane exposure. Results of interest include the following:
Of 56 million travelers screened
17,909 had fever and a respiratory illness
757 (14 per million) had influenza with the 2009 influenza A (H1N1) strain
Lab tests showed
C-reactive protein > 10 mg/L (31%)
Median CD4 count, 576 cells/µL
White blood cell (WBC) count > 10,000/mm3 (3%)
Mean WBC count, 3440/mm3
Total lymphocyte count, < 15,000/mm3 (68%)
Abnormal chest x-ray (5%) with "patchy infiltrates" in 12 of 14
Abnormal chest computed tomographic (CT) scan (7%)
Symptoms included
Fever (67%)
Cough (70%)
Sputum production (25%)
Sore throat (37%)
Diarrhea (3%)
Nausea (2%)
Viral shedding
Mean of 6 days by RT-PCR
Mean of 3 days after becoming afebrile
Longer with age < 14 years (odds ratio [OR] 1.94)
Longer with delayed oseltamivir treatment (> 48 hours after onset of symptoms [OR 4.5]).
Commentary. Extensive data of this type that are systematically collected in patients who are not very sick are difficult to find. Of note:
Viral shedding persisted an average of 3 days after the patients became afebrile;
Oseltamivir appeared to substantially reduce viral shedding if given within that 48-hour window after the onset of symptoms;
5% had patchy infiltrates on x-ray and 7% had abnormal chest CT scans;
Gastrointestinal symptoms were less common than reported in the US literature; and
Airport screening detected influenza in about 1 of 100,000 travelers.
Pediatric Hospitalizations Associated With 2009 Pandemic Influenza A (H1N1) in Argentina[9]
These investigators retrospectively reviewed the experience with 2009 H1N1 infections in 251 children from 6 pediatric hospitals in Buenos Aires. Highlights include the following:
42 of 251 children (17%) had respiratory syncytial virus coinfection;
Median patient age was 10 months, and 75% were ≤ 2 years of age and 60% were ≤ 1 year of age;
Oseltamivir was given within 48 hours of the onset of symptoms in only 11 of 251 (4%);
Suspected bacterial superinfection was present in 25 of 251 children (10%);
Intensive care unit admission was required in 41 (16%), mechanical ventilation in 42 (17%), and 13 died (5%);
Overall death rates in children were 10 times the rates in 2007: 2009, 1.1 of 100,000 children; 2008, 0 of 100,000 children; 2007, 0.1 of 100,000 children;
Death rate for infants < 1 year of age was 7.6 of 100,000; and
9 of 13 children (69%) who died had preexisting illnesses, especially asthma, chronic lung disease, or neurologic disease.
The investigators emphasized that this influenza was associated with an exceptionally high rate of respiratory failure and hypoxemic deaths in children, especially those < 1 year of age.
Viral shedding persisted an average of 3 days after the patients became afebrile;
Oseltamivir appeared to substantially reduce viral shedding if given within that 48-hour window after the onset of symptoms;
5% had patchy infiltrates on x-ray and 7% had abnormal chest CT scans;
Gastrointestinal symptoms were less common than reported in the US literature; and
Airport screening detected influenza in about 1 of 100,000 travelers.
Pediatric Hospitalizations Associated With 2009 Pandemic Influenza A (H1N1) in Argentina[9]
These investigators retrospectively reviewed the experience with 2009 H1N1 infections in 251 children from 6 pediatric hospitals in Buenos Aires. Highlights include the following:
42 of 251 children (17%) had respiratory syncytial virus coinfection;
Median patient age was 10 months, and 75% were ≤ 2 years of age and 60% were ≤ 1 year of age;
Oseltamivir was given within 48 hours of the onset of symptoms in only 11 of 251 (4%);
Suspected bacterial superinfection was present in 25 of 251 children (10%);
Intensive care unit admission was required in 41 (16%), mechanical ventilation in 42 (17%), and 13 died (5%);
Overall death rates in children were 10 times the rates in 2007: 2009, 1.1 of 100,000 children; 2008, 0 of 100,000 children; 2007, 0.1 of 100,000 children;
Death rate for infants < 1 year of age was 7.6 of 100,000; and
9 of 13 children (69%) who died had preexisting illnesses, especially asthma, chronic lung disease, or neurologic disease.
The investigators emphasized that this influenza was associated with an exceptionally high rate of respiratory failure and hypoxemic deaths in children, especially those < 1 year of age.
Commentary. Data from the United States showed that 2009 influenza A (H1N1) was responsible for an estimated 1090 deaths in children, far more than in in any of the 3 previous influenza seasons. This report from Argentina documents the same phenomenon—a 10-fold increase in mortality in children. The mortality rate in children <> 6 months of age, the need for vaccination among care providers of infants < 6 months of age, the importance of vaccine in pregnant women to protect both newborn and mother, and the importance of the new recommendations for oseltamivir in children.
H1N1 Influenza May Increase Maternal Deaths: Importance to Clinicians
A report of a study conducted in California[10] verified the high risk for severe disease among pregnant women and women who have just given birth who are infected with H1N1 influenza virus. Pregnant women accounted for nearly 10% of patients who have died or were hospitalized with H1N1 influenza.
H1N1 Influenza May Increase Maternal Deaths: Importance to Clinicians
A report of a study conducted in California[10] verified the high risk for severe disease among pregnant women and women who have just given birth who are infected with H1N1 influenza virus. Pregnant women accounted for nearly 10% of patients who have died or were hospitalized with H1N1 influenza.
Commentary. The major issues for clinical management of pregnant women with potential influenza are listed below:
Avoid delays in starting oseltamivir. Starting antiviral therapy more than 2 days after the onset of symptoms resulted in a 4.3-fold increase in mortality. In the women who died, the median length of time before oseltamivir was started was 6.5 days after the onset of symptoms.
Rapid tests for influenza are often falsely negative (38% false-negative rate), so antivirals need to be started on the basis of clinical features without reliance on the rapid test results.
Pregnancy is an acknowledged risk for bad outcome with influenza, but the 2009 influenza A (H1N1) has been unusually severe.
Pregnant women are a very high priority for vaccination and should be assured that this vaccine appears to be just as safe in pregnant women as in women who are not pregnant. The added benefit of vaccinating the mother is protection for her newborn infant in the 6 months between delivery and the time when the baby can be vaccinated.
Single Dose of H1N1 Vaccine Needed for Adults, 2 for Children
Randomized clinical trials of the safety and immunogenicity of pandemic H1N1 vaccines were recently conducted in the United States,[11] China,[12] and Hungary.[13] The new research confirms that a single dose of H1N1 vaccine is sufficient for adults, but not for many children.
Avoid delays in starting oseltamivir. Starting antiviral therapy more than 2 days after the onset of symptoms resulted in a 4.3-fold increase in mortality. In the women who died, the median length of time before oseltamivir was started was 6.5 days after the onset of symptoms.
Rapid tests for influenza are often falsely negative (38% false-negative rate), so antivirals need to be started on the basis of clinical features without reliance on the rapid test results.
Pregnancy is an acknowledged risk for bad outcome with influenza, but the 2009 influenza A (H1N1) has been unusually severe.
Pregnant women are a very high priority for vaccination and should be assured that this vaccine appears to be just as safe in pregnant women as in women who are not pregnant. The added benefit of vaccinating the mother is protection for her newborn infant in the 6 months between delivery and the time when the baby can be vaccinated.
Single Dose of H1N1 Vaccine Needed for Adults, 2 for Children
Randomized clinical trials of the safety and immunogenicity of pandemic H1N1 vaccines were recently conducted in the United States,[11] China,[12] and Hungary.[13] The new research confirms that a single dose of H1N1 vaccine is sufficient for adults, but not for many children.
Commentary. The new data have significance for practitioners. Influenza vaccine potency is determined by the serologic response rate that is conventionally defined as a hemagglutination titer of ≥ 1:40 at 21 days after vaccination. Response rates vary according to the antigen used, the dose, presence or absence of adjuvant (to boost the antigenic response), and the age of the recipient. These 3 trials support current US policy with regard to the following:
Response rates are good after single vaccine doses in persons > 9 years of age.
Children < 9 years of age require 2 doses, presumably because of lack of antigenic experience with flu and/or previous vaccine to this new strain.
The current policy was based on data in regard to the immunogenic response rates to vaccines without adjuvant. The decision was made for products in the United States to be unadjuvanted due to consumer concerns about the safety of adjuvants.
The bottom line is that the current policy is appropriate—a single dose for people > 9 years and 2 doses for children ≤ 9 years. The data are limited for seroresponse rates in high-priority groups in some studies, but most are not characterized by immunodeficiency so there is less concern that most of these groups would respond differently.
Sanofi Pasteur Recalls 800,000 Doses of Pediatric H1N1 Vaccine Due to Deficient Antigen Levels
Sanofi Pasteur recalled approximately 800,000 doses of its pediatric influenza A (H1N1) monovalent vaccine (single-dose, prefilled syringes) because antigen content was lower than required levels. The doses were part of 4 lots shipped in November and intended for children aged 6-35 months.
Response rates are good after single vaccine doses in persons > 9 years of age.
Children < 9 years of age require 2 doses, presumably because of lack of antigenic experience with flu and/or previous vaccine to this new strain.
The current policy was based on data in regard to the immunogenic response rates to vaccines without adjuvant. The decision was made for products in the United States to be unadjuvanted due to consumer concerns about the safety of adjuvants.
The bottom line is that the current policy is appropriate—a single dose for people > 9 years and 2 doses for children ≤ 9 years. The data are limited for seroresponse rates in high-priority groups in some studies, but most are not characterized by immunodeficiency so there is less concern that most of these groups would respond differently.
Sanofi Pasteur Recalls 800,000 Doses of Pediatric H1N1 Vaccine Due to Deficient Antigen Levels
Sanofi Pasteur recalled approximately 800,000 doses of its pediatric influenza A (H1N1) monovalent vaccine (single-dose, prefilled syringes) because antigen content was lower than required levels. The doses were part of 4 lots shipped in November and intended for children aged 6-35 months.
Commentary. Practitioners should be aware that:
The reduction in antigen in the recalled vaccine lots was modest, so children who received the vaccine probably had an antigenic response;
Revaccination of children vaccinated with recalled vaccine is not necessary; and
There are no safety issues with the recalled lots.
One 15-µg Dose of H1N1 Vaccine May Suffice in Infants and Children
In a study published in JAMA,[14] a single 15-µg dose of vaccine against the 2009 influenza A (H1N1) virus was safe and immunogenic in infants and children 6 months of age and older. The randomized, observer-blind, age-stratified, parallel-group study was conducted in Australia.
The reduction in antigen in the recalled vaccine lots was modest, so children who received the vaccine probably had an antigenic response;
Revaccination of children vaccinated with recalled vaccine is not necessary; and
There are no safety issues with the recalled lots.
One 15-µg Dose of H1N1 Vaccine May Suffice in Infants and Children
In a study published in JAMA,[14] a single 15-µg dose of vaccine against the 2009 influenza A (H1N1) virus was safe and immunogenic in infants and children 6 months of age and older. The randomized, observer-blind, age-stratified, parallel-group study was conducted in Australia.
Commentary. The reported study has limitations, and the data may not be applicable to all vaccine products. The current US policy of giving 2 doses of vaccine to children 6 months to 9 years of age should continue.
H1N1 Vaccine to Be Distributed Soon to Countries That Need It
In early 2010, Azerbaijan, Afghanistan, and Mongolia will be the first 3 countries to receive H1N1 influenza vaccine from donations made by manufacturers to the World Health Organization (WHO). In response to requests by WHO to donate vaccine supplies, 6 manufacturers in 12 countries agreed to provide a total of 180 million vaccine doses. These will be distributed to 95 countries that need vaccines. Countries in the northern hemisphere are the first targets for vaccine distribution because H1N1 activity remains high in those areas.
H1N1 Vaccine to Be Distributed Soon to Countries That Need It
In early 2010, Azerbaijan, Afghanistan, and Mongolia will be the first 3 countries to receive H1N1 influenza vaccine from donations made by manufacturers to the World Health Organization (WHO). In response to requests by WHO to donate vaccine supplies, 6 manufacturers in 12 countries agreed to provide a total of 180 million vaccine doses. These will be distributed to 95 countries that need vaccines. Countries in the northern hemisphere are the first targets for vaccine distribution because H1N1 activity remains high in those areas.
Commentary. The primary responsibility of most governments is to protect its citizens. Thus, the countries that can afford to make or buy vaccine will use most of it for its own population. The policy of the United States has been to allocate10% of its vaccine supply to resource-limited countries. WHO plans to give each country enough vaccine to protect 10% of its population, with the first 2% targeted to healthcare workers. To put these figures into perspective, the current US vaccine supply is about 110 million doses, enough to vaccinate about 35% of the population. Total use to date is estimated at 60 million doses or about 20% of the US population.